Physician Credentialing & Insurance Enrollment Services
Professional Medical Provider Credentialing & Insurance Enrollment Services
Medical credentialing and insurance enrollment can be a major challenge for providers and physicians due to its complexity and time-consuming nature. Without proper enrollment, insurance carriers may delay or refuse payment, leading to significant lost income. Medical credentialing services and insurance credentialing for physicians ensure that your practice runs smoothly and efficiently.
At Microwize, we offer medical credentialing services to help providers simplify their process & achieve better revenues. Contact us to get started!
What is Credentialing & Why Do Doctors Need It?
Physician credentialing is the process of enrolling and validating a physician as a member of a payer’s network, authorizing them to provide services to patients. Credentialing is essential to ensure that the physician meets the standards set by the payer (insurance company). This involves reviewing various aspects such as the physician’s license, experience, certification, education, training, affiliations, malpractice history, adverse clinical occurrences, and clinical judgment.
When Do Physicians Need Credentialing?
• When starting to practice after medical school
• When enrolling with a new payer
• When adding new provider to an existing group
• When forming a new group
• When starting a new practice
• When changing from one practice to another
Providers We Serve:
• Physicians (MDs or DOs)
• Pediatricians
• Physician Assistants (PAs)
• Nurse Practitioners (NPs)
• Physical Therapists (PTs)
• Occupational Therapists (OTs)
• Speech-Language Pathologists (SLPs)
• Podiatrists (DPMs)
• Chiropractors (DCs)
• Ambulatory Surgery Centers (ASC)
• Urgent Care Facilities
• Diagnostic Testing Facilities (IDTF)
• Sleep Labs
• Optometrists
• Audiologists
• Behavioral Health Providers
Medical Credentialing for Physicians – Pricing Information & Cost Breakdown
Frequently Asked Question (FAQ)
How Long Does the Physician Credentialing Process Take?
The average processing time for a new enrollment is 90 days.
After submission, we follow up on the application every 3 weeks until completion. Despite the requests from offices, daily outreach to the insurance company will not will not speed up the enrollment process.
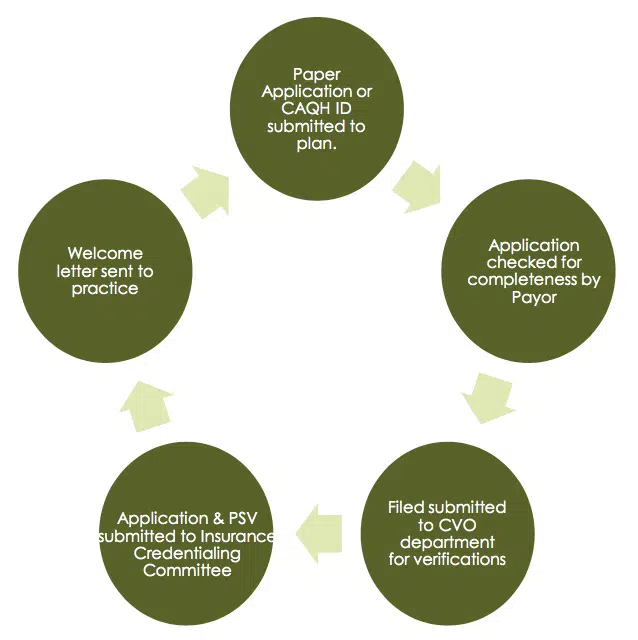
- Paper Application or CAQH ID submitted to plan.
- Welcome letter sent to practice
- Application checked for completeness by Payor
- Once Par IDs have been obtained, they are reported back to the office via a PAR ID
What Services are Included in the Contract?
Because we are a full service provider enrollment company. Included in our pricing model are the following:
- All Provider Initial and Recred enrollments
- Medicaid and Medicare Enrollments
- CAQH Set-up & Maintenance
- Provider location updates/moves
- Verification of providers enrollments (done during onboarding and as issues arise)
- Provider Demographic Verifications (from payers)
Steps in Provider Credentialing

Discussion of project, establish governance structure and contacts as well as meeting times & frequency, onboarding forms, reporting needs, etc.


 Audit of CAQH
Audit of CAQH
Filling in of any enrollment gaps via application or link

Ongoing communication to customer of Par IDs and completed enrollments
Insurance Enrollment Credentialing Services With
Commercial Insurance:
• Aetna
• Cigna
• Anthem
• Blue Cross Blue Shield (BCBS)
• TriCare
• Humana
• UnitedHealthcare
• Oxford
& many more…
Governmental Payers:
• Medicare
• Medicare Part B
• Railroad Medicare
• Medicaid
Initial Registration and Re-validation:
• PECOS
• CAQH Registration
•NPI Registration
Medical Credentialing Services Include
- Applications and forms state license verification
- DEA verification
- NPI verification
- OIG exclusion list
- ABMS verification
- Background checks
- AMA profiles delineation of privileges (DOPs)
- Certificates of Insurance (COIs)
- ECFMG confirmations peer reference verification facility verification educational verification
Ask us about the full RCM service Medical Billing Service