 Centers for Medicare and Medicaid Services (CMS) recently conducted a week long test wherein 660 volunteer Medicare fee-for-service providers, clearing houses and billing companies submitted about 15,000 test claims, and Administrator Marilyn Tavenner says CMS is ready. Of the claims submit 56% were from professionals, 38% were from institutions and 6% were supplier claims.
Centers for Medicare and Medicaid Services (CMS) recently conducted a week long test wherein 660 volunteer Medicare fee-for-service providers, clearing houses and billing companies submitted about 15,000 test claims, and Administrator Marilyn Tavenner says CMS is ready. Of the claims submit 56% were from professionals, 38% were from institutions and 6% were supplier claims.
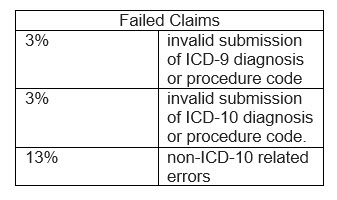
The goal of the test is to have providers successfully submit claims using ICD-10 codes to the Medicare Fee-For Service (FFS) claims systems, to see that CMS software changes resulted in appropriately adjudicated claims, and to make sure that accurate remittance occurs and results showed 81% of claims being accepted. And of the failed claims, many of the failures did not have to do with the ICD coding at all; they were rejected for other issues. Of the failures:
Marilyn Tavenner stated, “This successful week of testing continues to put us on course for successful implementation of this important initiative that better reflects modern practice of medicine by Oct. 1.” While CMS is calling the test a success, some are saying it would be catastrophic if CMS sees the same 19% failure rate on the October 1 deadline as it did during this first testing round.
This was just the first of 3 testing periods. But even with more testing on the horizon, just 21% of physician practices (according to the third ICD-10 readiness survey, published by Navicure and Porter Research) say they’re on track with their preparations for the switch to the new codeset.
With Medisoft, your ICD-10 transition can be smooth. To beat the last-minute rush and prevent any interruption to your practice’s cash flow, please contact Microwize Technology at 800-955-0321 for information on Medisoft practice management software.
